Caroline Costongs, Director of EuroHealthNet, reviews the latest evidence on whether European countries are on track to reach goals on reducing the burden of non-communicable diseases (NCDs). While the EU has certainly made progress, the NCD reduction rate is slowing down. What are initiatives taken at the European and international level to accelerate action?
Time flies and only 8 years remain to achieve the targets of the UN 2030 Agenda for Sustainable Development. Will European countries reach Sustainable Development Goal (SDG) number 3, “ensuring healthy lives and promoting wellbeing for all at all ages”? The pandemic has affected progress and introduced many competing health priorities. Thus, it is important to take time to evaluate and assess our improvements in health – before it’s too late.
SDG 3 has several targets, including target 3.4 aimed at reducing non-communicable diseases (NCDs). NCDs are the leading causes of ill health worldwide and were responsible for seven out of ten premature deaths in 2019 (WHO 2022).
Under target 3.4, countries have committed to, by 2030, reduce by one-third premature mortality from NCDs, through prevention and treatment, and promote mental health and wellbeing. Progress is evaluated using two indicators:
3.4.1 Mortality rate attributed to cardiovascular disease, cancer, diabetes or chronic respiratory disease
3.4.2 Suicide mortality rate

How are we doing on the NCD indicator 3.4.1.?
The WHO and the European Union (EU) have recently published their SDG monitoring reports (WHO 2022, Eurostat 2022). Unfortunately, most of the data is from before COVID-19 and therefore doesn’t capture the full impacts of the pandemic. The actual state of NCDs in Europe thus is expected to be worse than reported, as emerging evidence tells us that the pandemic aggravated the existing NCD burden, as well as some of its determinants and risk factors and has disrupted NCD care services.
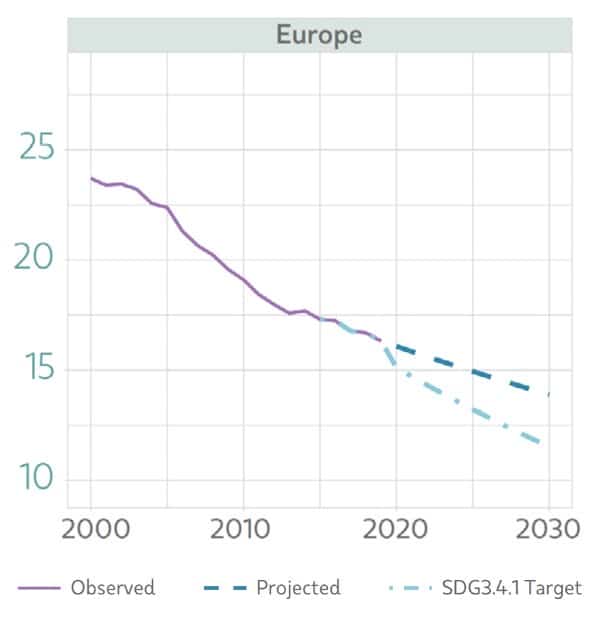
However, even if we look at the pre-pandemic data, the situation does not seem good. Due to improved prevention, diagnosis and treatment we see a significant decrease in global premature NCD mortality, with the greatest decline in the WHO European region over the past two decades. But, despite this progress, the pace of change in most countries is too slow to achieve SDG target 3.4. According to the World Health Organisation, at the current pace of improvement, SDG target 3.4 will not be met by 2030 (WHO 2022).
What about the European Union, how close are we to meeting the SDG3 NCD target?
In the EU, the “probability of dying between the ages of 30 and 70 years from cardiovascular diseases, cancer, diabetes, or chronic respiratory diseases” decreased from 15.8% in 2010 to 13.4% in 2019 (The Global Health Observatory, 2022). While this represents an average reduction of 1.9%, the actual pace of progress has steadily declined in recent years. Based on our estimates, pre-mature mortality due to NCDs will only have been reduced by 23% by the year 2030, compared to 2015. This is 10% less than the targeted 33%, meaning that the EU is also not on track.
The 2022 Eurostat report tells us that trends in risk factors are mixed. For instance, while the share of smokers has declined, which may partly explain the decrease in NCDs, the share of obese and overweight people has grown in the EU. In 2019, more than half of Europeans above the age of 18 were overweight or obese, an alarming statistic. In addition, these rates are linked to significant health inequalities: obesity rates range from 11.4% for people with tertiary education to 20.3 % for people with lower secondary education or lower. Big differences are also found between EU Member States, with values ranging from 10.9% to 28.7% for obese people over the age of 18 (Eurostat 2022).
As the world is off track, the May 2022 World Health Assembly approved a range of NCD measures and an important global implementation road map to accelerate action on noncommunicable diseases (2023-30). The European Commission followed suit, and launched its first ever NCD initiative “Healthier Together” (2022-27) in June 2022.
The new EU NCD initiative - what is it?
The NCD initiative is key to help us speed up our actions. It consists of an extensive toolkit to guide EU countries in identifying their priorities and implementing effective measures to reduce NCDs and improve citizens’ health and wellbeing. It provides valuable information and concrete recommendations for action. The initiative covers cardiovascular diseases, diabetes, chronic respiratory diseases and mental health. Cancer is covered through Europe’s Beating Cancer Plan.

The NCD initiative is supported by ambitious funding from the EU4Health programme. It aims to implement actions on the ground and select interventions that could benefit from EU funding to achieve faster and wider deployment. It also aims to reduce health inequalities within and between EU Member States. But will this be enough to tackle the NCDs and trends mentioned above?
NCDs cost EU economies €115 billion, or 0.8% of GDP, annually in addition to other associated societal costs, such as loss of workforce, productivity and costs of social care. In that sense, we need ambitious, structured and systemic change at EU and national levels to reduce the €115 billion cost of ‘repair’.
The EU and Member States need to provide and support a truly strategic approach across sectors and government that includes action on the underlying determinants of NCDs (such as poverty, social protection, and the commercial determinants of health) and has clear measurable objectives. As EuroHealthNet stressed in its latest statement about the EU NCD initiative, the initiative is extremely helpful when complemented by strong coordination at EU and Member State levels and an integrated approach to tackling NCDs in efforts to build resilient health systems.
Public health, health promotion and disease prevention are an essential part of such a structured approach. They have so much to contribute to improving our health and wellbeing, as evidenced by the wide range of articles in this edition of our magazine. The profiled initiatives and approaches positively impact on the determinants of ill health and directly reduce incidence and prevalence of NCDs. I am therefore truly delighted to share another excellent edition with you, covering crucial work from the EuroHealthNet Partnership.

Investing in health throughout the life-course
In Spain, the Andalusian Comprehensive Strategy for the Promotion of Healthy Living (currently being drafted) takes a much-needed intersectional and holistic approach to health promotion, taking on board views of businesses, civil society and individuals.
In Wales, the Adverse Childhood Experiences (ACEs) Hub protects children’s wellbeing by preventing and mitigating abuse and other traumatic events, breaking the long-term and often inter-generational cycle of ACEs, adversity, and trauma across the life-course.

An article summarising the EuroHealthNet 2022 seminar reflects lessons learnt, including the value of investing in comprehensive school-based health promotion programmes and correcting misperceptions about the impacts of an ageing population on the economy.


Social prescribing
Over recent years, social prescribing has emerged as a health-promoting practice that enables primary care providers to connect people to community support in order to improve health and wellbeing. Luciana Costa of the Portuguese National Institute of Health Doutor Ricardo Jorge (INSA) shares with us a personal account of EuroHealthNet’s Country Exchange Visit, speaking about the value of social prescribing, personal enlightenment and the importance of intersectoral approaches.
In Austria, where every fifth consultation in primary care is due to health-related, but non-medical concerns, a project run by the Austrian National Public Health Institute supported nine facilities as they experimented with social prescribing. Meanwhile, the European project Culture4Health aims to facilitate the exchange of knowledge and success stories related to the role of culture in supporting wellbeing and health.
Green and public spaces
Housing circumstances and access to green spaces are important not only to prevent NCDs but support overall wellbeing. In Latvia’s capital city, Riga, a Development Programme 2022-2027 aims to meet the challenges posed by climate change, prioritising environmentally-friendly commuting within the city, improving access to health care and social support, and ensuring a resilient urban ecosystem.
By applying a ‘placemaking’ approach, Wales aims to shape environments through the lens of health and wellbeing, and to support communities that enable people to make healthier lifestyle choices, prevent illness, address inequalities, and improve access to services and facilities.



Access and discrimination in healthcare
While health care is a basic and universal need, some groups still face barriers and discrimination, often due to discrimination and misunderstanding or lack of interest of health professionals in their patients’ backgrounds. In the Netherlands, Pharos strives to improve healthcare for people with migration backgrounds, and reduce health disparities between between people with a higher and lower socioeconomic status and different migration backgrounds by providing guidance for healthcare institutions.
(Undocumented) migrants can face particular difficulty accessing healthcare, as they are often not familiar with the health system, and face discrimination and fear of repercussions for contacting authorities. In Southern Italy, the FARI project provides information and helps foreign communities to navigate the system of health and social services, promoting the universal right to care.
Please let us know what you think of this Magazine. EuroHealthNet will continue to search for, collect and share examples of policy, practices and promising research findings that have an impact on health and wellbeing, including reducing NCDs. We are keen to help implement the EU NCD initiative and help to meet SDG 3 by 2030. If you have any practices or innovations to share, do not hesitate to get in touch.

Caroline Costongs
Caroline Costongs is Director of EuroHealthNet and expert in public health and health promotion. Caroline leads a multi-disciplinary team working on European and (sub)national policy, advocacy, research and capacity building addressing health inequalities. Caroline is active in various EU and WHO fora, Advisory Boards and various EU projects, and is a member of the ICC – International Council for the European Public Health Conference.